Abstract
Introduction -primary refractory AML is associated with a dismal prognosis with only 30% of the patients responding to salvage chemotherapy and continuing to allogeneic hematopoietic cell transplantation (HCT). HCT with a standard myeloablative conditioning regimen ,given to patients with a primary refractory leukemia,is associated with 10-20% long- term overall survival. The fludarabine, amsacrine, and cytarabine (FLAMSA)-reduced-intensity conditioning (TBI-based or treosulfan-based) protocol, established by the German group, has been described to be effective approach in patients with relapse/refractory AML undergoing HCT. Modified protocol (without amsacrine and with TBI-based RIC, FITCy) has been also used in the last several years.
Methods - We retrospectively analyzed the HCT characteristics and outcomes of all consecutive patients ,diagnosed with primary refractory AML who underwent HCT with either the FLAMSA or FITCy regimens in the University of Cologne and the Tel Aviv Medical Center. Patients who underwent sequential therapy for relapsed disease (either chemosensitive or refractory) were excluded from this analysis.
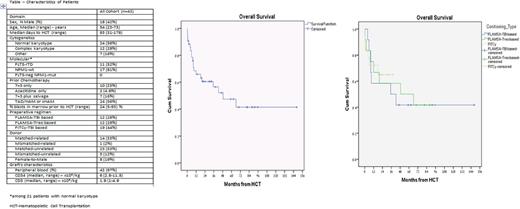
Results - Between the years 2003 and 2017, we identified 43 patients that were eligible for this analysis. Median age was 54 (range, 23-73) years (Table). Median follow-up for surviving patients was 32 (range, 1-148) months. Twelve patients (28%) received only one line of chemotherapy (mostly 7+3) before proceeding at a refractory state to HCT. Preparative regimens were FLAMSA-TBI based, FLAMSA-Treo based and FITCy in 12 (28%), 12 (28%), and 19 (46%) patients, respectively. Prior to HCT, 5 (12%) patients had ongoing documented infections (either microbiology or clinically) - aspergilus pneumonia (n=3), atypical pneumonia (n=1), and scrotal abscess (n=1). Median days to engraftment of neutrophils (>500/dL) and to incomplete engraftment of platelets (>20000/dL) were 13 (range, 9-19) days, and 13 (7-30) days, respectively. Only 1 patient (2%) had primary graft rejection. Severe mucositis was observed in only 10% of the patients, and was mostly observed in the upper gut. 3 patients (7%) developed fungal pneumonia and 2 patients (5%) had blood stream infection during the neutropenic period. Only 2 patients (5%) developed sinusoidal obstruction syndrome.
Complete remission was documented on day 30, in all but 1 patient. Cumulative incidences of grade 2-4 and 3-4 acute GVHD at day 100 were 40% and 20%, respectively. Cumulative incidences of overall chronic GVHD and moderate-severe chronic GVHD at 1 year after HCT were 76% and 52%, respectively. Cumulative incidences of relapse at 1 year and 2 years post HCT were 22% and 25%, respectively. Non-relapse mortality rates, at 30 days, 100 days and 1 year post HCT were 7%, 10%, and 22%, respectively. Cumulative incidences of 1, 2,and 3 years overall survival were 66%, 60%, and 57% , Figure. Both older age and a mismatched donor were associated with decreased overall survival (HR=0.83, 95% CI=.335-.969, p=.02) and (HR=.25, 95% CI=.064-.954, p=.046), while time from 1st line regimen to HCT, uncontrolled infections at HCT, percentage of BM blasts prior to HCT, and type of the preparative conditioning were not predictive for survival.
Conclusions - Sequential therapy in patients with primary refractory AML is safe and provides a remarakablre anti- leukemic effect. In patients with available donors, this strategy may be superior to repeating rounds of salvage chemotherapy and should be further studied in other settings (i.e. haploidentical donors and other diseases). Future protocols should focus on decreasing GVHD rate , maintaining the graft vs. leukemia effect.
Scheid: BMS: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria; Takeda: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal